 Lymphodema
Lymphodema
Lymphedema symptoms and causes
________________________________________________________________________________________________________
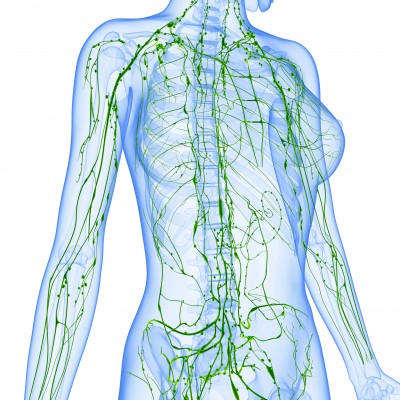
The lymphatic system
Immune system cells circulate through the bloodstream or the lymphatic system.
The body has approximately 600 lymph nodes, but only those in the submandibular, axillary or inguinal regions may normally be palpable in healthy people. The lymphatic system is an extensive drainage tubes (or vessels) that helps keep bodily fluid levels in balance and defends the body against infection.
It is a network of tubes throughout the body that drains fluid (called lymph) from tissues and empties it back into the bloodstream. It acts like a vacuum system.
The main roles
Lymph is filtered through the spleen, thymus and lymph nodes before being emptied into the blood.
Keeping a balance of fluid
Blood vessels tend to seep fluid into surrounding tissue. The lymphatic system drains off any extra fluid to stop the tissues from puffing up. The feet in particular are prone to puffiness. Also for people who had lymph nodes removes
- It is responsible for the removal of interstitial fluid from tissues
- It absorbs and transports fatty acids and fats as chyle from the digestive system
- It transports white blood cells to and from the lymph nodes into the bones
- The lymph transports antigen-presenting cells (APCs), such as dendritic cells, to the lymph nodes where an immune response is stimulated.
______________________________________________________________________________________________________________
Cancer
The study of lymphatic drainage of various organs is important in diagnosis, prognosis, and treatment of cancer. The lymphatic system, because of its physical proximity to many tissues of the body, is responsible for carrying cancerous cells between the various parts of the body in a process called metastasis. The intervening lymph nodes can trap the cancer cells. If they are not successful in destroying the cancer cells the nodes may become sites of secondary tumors.
______________________________________________________________________________________________________________
Lymphatic vessels
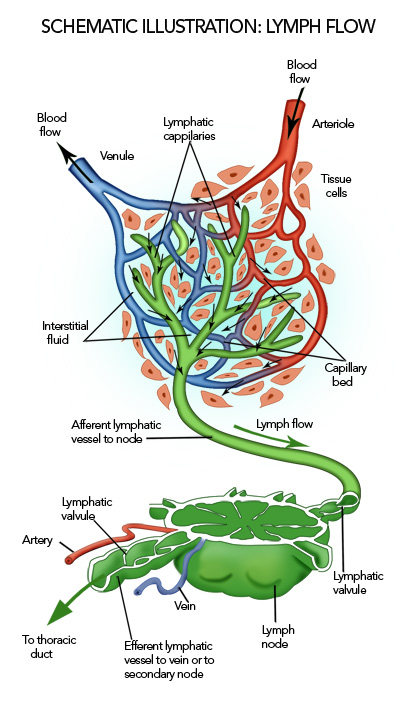 Lymphatic vessels run in your the entire body, except for the central nervous system. Some lymphatic vessels have valves (similar to the valves in veins), which stop from running back the wrong way.
Lymphatic vessels run in your the entire body, except for the central nervous system. Some lymphatic vessels have valves (similar to the valves in veins), which stop from running back the wrong way.
Lymphedema may be inherited (primary) or caused by injury to the lymphatic vessels (secondary). It is most frequently seen after lymph node dissection, surgery and/or radiation therap, in which damage to the lymphatic system is caused during the treatment of cancer, most notably breast cancer. In many patients with cancer this condition does not develop until months or even years after therapy has concluded.
Lymphedema may also be associated with accidents or certain diseases or problems that may inhibit the lymphatic system from functioning properly.In tropical areas of the world, a common cause of secondary lymphedema is filariasis, a parasitic infection. It can also be caused by a compromising of the lymphatic system resulting from cellulitis.
While the exact cause of primary lymphedema is still unknown, it generally occurs due to poorly developed or missing lymph nodes and/or channels in the body. Lymphedema may be present at birth, develop at the onset of puberty (praecox), or not become apparent for many years into adulthood (tarda). In men, lower-limb primary lymphedema is most common, occurring in one or both legs. Some cases of lymphedema may be associated with other vascular abnormalities.
Secondary lymphedema affects both men and women. In women, it is most prevalent in the upper limbs after breast cancer surgery and lymph node dissection, occurring in the arm on the side of the body in which the surgery is performed. Head and neck lymphedema can be caused by surgery or radiation therapy for tongue or throat cancer. It may also occur in the lower limbs or groin after surgery for colon, ovarian or uterine cancer in which removal of lymph nodes or radiation therapy is required. Surgery and/or treatment for prostate, colon and testicular cancers may result in secondary lymphedema, particularly when lymph nodes have been removed or damaged.
Lymph nodes A lymph node is an organized collection of lymphoid tissue, through which the lymph passes on its way to returning to the blood. Lymph nodes are located at intervals along the lymphatic system. Several afferent lymph vessels bring in lymph, which percolates through the substance of the lymph node, and is drained out by an efferent lymph vessel. Lymph nodes are particularly numerous in the mediastinum in the chest, neck, pelvis, axilla (armpit), inguinal (groin) region, and in association with the blood vessels of the intestines.
The onset of secondary lymphedema in patients who have had cancer surgery has also been linked to aircraft flight (likely due to decreased cabin pressure). For breast cancer survivors, wearing a prescribed and properly fitted low-compression sleeve and gauntlet may help decrease swelling during flight.
Some cases of lower-limb lymphedema have been associated with the use of tamoxifen, due to the blood clots and deep vein thrombosis (DVT) that can be caused by this medication. Resolution of the blood clots or DVT is needed before lymphedema treatment can be initiated.
_______________________________________________________________________________________________________________
Lymphedema Symptoms and Causes
- Swelling worsens over time
- Repeated episode of infection
- Sensation of heaviness and limited motion
- Clothes, jewelry or shoes no longer fit
Possible Causes of Lymphedema
- Treatment of cancer
- Birth defects
- Infections
- Trauma (injury or surgery)
- Circulatory disorders
General Recommendations
- Protect the area below the surgery from injury, even many years after surgery.
- If you have had lymph nodes removed from under your arm
- Do not have blood drawn from the arm on the side of the lymph node surgery.
- Do not allow a blood pressure cuff to be placed on that arm. If you are in the hospital, make sure you notify your nurse and other hospital staff of your condition.
- Avoid razors, use an electric shaver for underarms.
- Wear gloves when gardening or doing other activities that may lead to cuts on your fingers or hands.
- Wear strong sunscreen to avoid sunburn.
- Practice good skin care to reduce the risk of infection
- It is important to keep your weight within normal limits as much as possible.
_______________________________________________________________________________________________________________
Diagnosis
Assessment of the lower extremities begins with a visual inspection of the legs. Color, presence of hair, visible veins, size of the legs and any sores or ulcerations should be noted.
Lack of hair may indicate an arterial circulation problem.
If swelling is observed, the calf circumference should be measured with a tape measure. This measurement can be compared to future measurements to see if the swelling is getting better. Determine if elevating the legs makes the swelling go away. Pressure should be applied with the fingertips over the ankle to determine the degree of swelling.
The assessment should also include a check of the popliteal, femoral, posterior tibial, and dorsalis pedis pulses. When checking the femoral pulse, feel for the inguinal nodes and determine if they are enlarged. Enlargement of the nodes lasting more than three weeks may indicate infection or some other disease process requiring further medical attention.
The diagnosis or early detection of lymphedema is difficult. The first signs may be subjective observations such as “my arm feels heavy” or “I have difficulty these days getting rings on and off my fingers”. These may be symptomatic of early stage of lymphoedema where accumulation of lymph is mild and not detectable by any difference in arm volume or circumference (see severity above).
As lymphedema develops further, definitive diagnosis is commonly based upon an objective measurement of difference between the affected or at-risk limb at the opposite unaffected limb, e.g. in volume or circumference. Unfortunately, there is no generally accepted worldwide criterion of difference definitively diagnostic although a volume of difference of 200 ml between limbs or a 4 cm (at a single measurement site or set intervals along the limb) is often used.
Recently the technique of bioimpedance measurement (a method that measures the amount of fluid in a limb) has been shown to have greater sensitivity than these existing methods and holds promise as a simple diagnostic and screening tool.Impedance analysers specifically designed for this purpose are now commercially available.
_______________________________________________________________________________________________________________
Whether primary or secondary, lymphedema develops in stages, from mild to severe. Methods of staging are numerous and inconsistent. They ranged from three to as many as eight stages.
The most common method of staging was defined by the Fifth WHO Expert Committee on Filariasis:
- Stage 0 (latent): The lymphatic vessels have sustained some damage which is not yet apparent. Transport capacity is still sufficient for the amount of lymph being removed. Lymphedema is not present.
- Stage 1 (spontaneously reversible): Tissue is still at the “pitting” stage: when pressed by the fingertips, the affected area indents and holds the indentation. Usually upon waking in the morning, the limb or affected area is normal or almost normal in size.
- Stage 2 (spontaneously irreversible): The tissue now has a spongy consistency and is considered “non-pitting:” when pressed by the fingertips, the tissue bounces back without any indentation. Fibrosis found in Stage 2 Lymphedema marks the beginning of the hardening of the limbs and increasing size.
- Stage 3 (lymphostatic elephantiasis): At this stage, the swelling is irreversible and usually the limb(s) or affected area is very large. The tissue is hard (fibrotic) and unresponsive; some patients consider undergoing reconstructive surgery called “debulking”. This remains controversial, however, since the risks may outweigh the benefits, and the further damage done to the lymphatic system may in fact make the lymphedema worse.
 A new staging system has been set forth by Lee, Morgan and Berganand endorsed by the American Society of Lymphology. This provides a clear technique which can be employed by clinical and laboratory assessments to more accurately diagnose and prescribe therapy for lymphedema. In this improved version there are four stages identified (I-IV). Physicians and researchers can use additional laboratory assessments such as bioimpedance, MRI, or CT to build on the findings of a clinical assessment (physical evaluation). From this, results of therapy can be accurately be determined and reported in documentation as well as research.
A new staging system has been set forth by Lee, Morgan and Berganand endorsed by the American Society of Lymphology. This provides a clear technique which can be employed by clinical and laboratory assessments to more accurately diagnose and prescribe therapy for lymphedema. In this improved version there are four stages identified (I-IV). Physicians and researchers can use additional laboratory assessments such as bioimpedance, MRI, or CT to build on the findings of a clinical assessment (physical evaluation). From this, results of therapy can be accurately be determined and reported in documentation as well as research.
Risk is another measurement altogether. Current research using bioimpedance to measure risk of lymphedema is very promising.
_______________________________________________________________________________________________________________
Treatment
Treatment for lymphedema varies depending on the severity of the edema and the degree of fibrosis of the affected limb. Most people with lymphedema follow a daily regimen of treatment as suggested by their physician or certified lymphedema therapist.
The most common treatments for lymphedema are a combination of the daily use of intermittent sequential multi-chambered overlapping gradient pumps, manual compression lymphatic massage, compression garments or bandaging.
Complex decongestive physiotherapy is an empiric system of lymphatic massage, skin care, and compressive garments. Although a combination treatment program may be ideal, any of the treatments can be done individually.
_______________________________________________________________________________________________________________
Common problems
Certain diseases can affect the lymph nodes, the spleen, or the collections of lymphoid tissue in certain areas of the body.
Some common problems of the lymphatic system include:
Glandular fever – symptoms include tender lymph nodes, Glandular Fever is a viral infection caused by the Epstein-Barr virus. Glandular Fever is often spread through oral acts such as kissing, which is why it is sometimes called “The Kissing Disease”. However, Glandular Fever can also be spread by airborne saliva droplet. Very little can be done to treat Glandular Fever. The symptoms usually pass over the space of about two to four weeks without any complications.
Hodgkin’s disease – is a cancer of the lymphatic system, also known as a lymphoma. It is one of many kinds of cancers of the lymphatic system.
Oedema – swelling caused by too much fluid in the tissues is the build-up of fluid in the body which can cause swelling in the arteries. In many cases the oedema swells to an extent which causes it to be visible outside the skin. Oedema mainly affects the arms and legs, including the hands, ankles and feet.
Tonsillitis – infection of the tonsils in the throat. It is a disease. The tonsils in the mouth get inflamed, and grow red. This may cause a sore throat or a fever. Usually the inflammation goes away with time, but if it does not the tonsils may have to be surgically removed. This operation is called a tonsillectomy. The disease is caused by certain viruses most of the time, but can also be caused by bacteria. It easily spreads between humans. The most important thing is to treat sore throat (pharyngitis) if, it is caused by bacteria called streptococcus, you will need antibiotic for a few days.
Lymphadenopathy – It’s a term meaning “disease of the lymph nodes. This is where the lymph nodes become swollen or enlarged; it also can be abnormal in either size, consistency or number. When a person is experiencing a virus, cold or infection usually they notice the “glands” in their neck may be swollen. This is part of the bodies’ immune response to any type of foreign invader. It can be due to infection, auto-immune disease, or malignancy. Lymph nodes greater than 1 cm in diameter are considered to be abnormal. The condition is classified as localized if node enlargement is limited to one area. If two or more areas are affected it is referred to as generalized lymphadenopathy.
Lymphadenitis. Also called adenitis, this inflammation or enlargement of the lymph node is caused by an infection of the tissue in the node. The infection can cause the skin overlying the lymph node to swell, redden, and feel warm and tender to the touch. Lymphadenitis may affect a single node or a group of nodes (regional adenopathy) and may be unilateral or bilateral. This infection usually affects the lymph nodes in the neck, and it’s usually caused by a bacterial infection that can be easily treated with an antibiotic. The onset and course of lymphadenitis may be acute, subacute, or chronic. Lymphadenitis may spread within hours. Treatment should begin promptly.
Lymphomas – Lymphoma is a cancer of the lymphocytes, a type of cell that forms part of the immune system. These cancers start in the lymph nodes when lymphocytes undergo changes and start to multiply out of control. The lymph nodes swell, and the cancer cells crowd out healthy cells and may cause tumors (solid growths) in other parts of the body. Treatment might involve chemotherapy and in some cases radiotherapy and/or bone marrow transplantation, and can be curable depending on the histology, type, and stage of the disease. It can also affect other organs in which case it is referred to as extranodal lymphoma. Extranodal sites include the skin, brain, bowels and bone. Lymphomas are closely related to lymphoid leukemias, which also originate in lymphocytes but typically involve only circulating blood and the bone marrow.
Splenomegaly (enlarged of the spleen) – The spleen usually lies in the left upper quadrant of the human abdomen. The spleen is usually small enough that it can’t be felt when you press on the abdomen. Certain diseases can cause the spleen to swell to several times its normal size. Moderate splenomegaly, if the largest dimension is between 11–20 cm. Severe splenomegaly, if the largest dimension is greater than 20 cm.
Usually, this is due to a viral infection, such as mononucleosis. more serious diseases such as cancer cells from a hematological malignancy and portal hypertension can cause it to expand. It is not surprising that splenomegaly is associated with any disease process that involves abnormal red blood cells being destroyed in the spleen. Splenomegaly may also come from bacterial infections, such as syphilis or an infection of the heart’s inner lining. Doctors usually tell someone with an enlarged spleen to avoid contact sports like football for a while because a swollen spleen is vulnerable to rupturing (bursting). And if it ruptures, it can cause a huge amount of blood loss.
_______________________________________________________________________________________________________________
ASSOCIATIONS
CANADA
http://www.lymphovenous-canada.ca/groups1.htm
The Klippel-Trenaunay Group is a world-wide organization which has a number of Canadian members. http://k-t.org/
BRITISH COLUMBIA
ALBERTA
http://www.albertalymphedema.com
SASKATCHEWAN
Contact Eunice Mooney, president at: 306-922-0851
MANITOBA
Contact Kim Avanthay at: mailto:kimavant@mymts.net
ONTARIO
Note: Several Ontario lymphedema support groups have been established across Ontario through the efforts of the LAO (great work!)
Kingston Lymphedema Support Group, established under the auspices of Breast Cancer Action Kingston, 613-531-7912 or visit their website at: http://wwww.bcakingston.org
North Bay Lymphedema Education and Support Group. For more information call Susan Woodman at: 705-497-0683
Oshawa Lymphedema Support Group, at the Hearth Place Cancer Support Centre, 905-579-4833
Breast Cancer Action Ottawa , 613-736-5921. BCA Ottawa received a Community Health Promotion grant from the Canadian Breast Cancer Foundation to undertake a two year outreach project which includes lymphedema-related exercise and education. The LAO is a member of its project steering committee. For information on dates and times for this group call: 613-736-5921
Toronto Lymphedema Information and Support Group, at Sunnybrook Health Sciences Centre, sponsored by the LAO in connection with Wellspring. For more information and to register call LAO at: 416-410-2250 or toll free at: 877-723-0033
QUEBEC
AQL/LAQ
Mailing address: 6565 St. Hubert, Montréal, QC H2S 2M5
Telephone number: 514-979-2463
http://www.infolympho.ca/en/index.en.htm
http://www.infolympho.ca/fr/index.fr.htm
NEW BRUNSWICK/YUKON
Support Group, is leading up this initiative and can be reached at: mailto:sophied@rrsb.nb.ca.
NOVA SCOTIA
Support Group, is leading up this initiative and can be reached at: mailto:sophied@rrsb.nb.ca.
PEI/LABRADOR
Joyce can be reached at: mailto:joyce8184@gmail.com
NEWFOUNDFLAND
You can contact Bev for more information at: mailto:bev.lanning@centralhealth.nl.ca
NORTHWEST TERRITORIES
So far nothing! Check at you local Hospital
US
National Lymphedema Network, http://www.lymphnet.org
StepUp-SpeakOut www.stepup-speakout.org
Lymph Notes www.lymphnotes.org
Lymphovenous Canada www.lymphovenous-canada.ca
Lymphedema Support Network www.lymphoedema.org/Isn (Britain)
Lymphoedema Network Australia www.lymphoedema.org.au
_______________________________________________________________________________________________________________





